What’s wrong with this picture; I see what you mean; I hear where you’re coming from; Something doesn’t feel right:
These statements represent analytics.
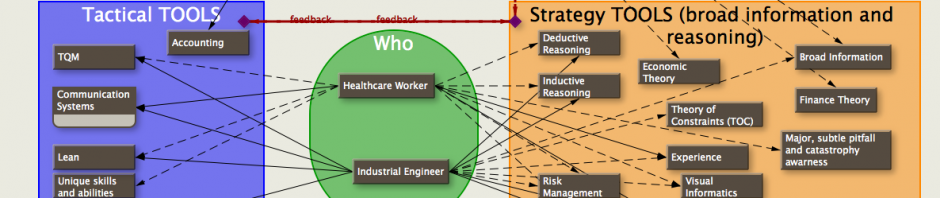
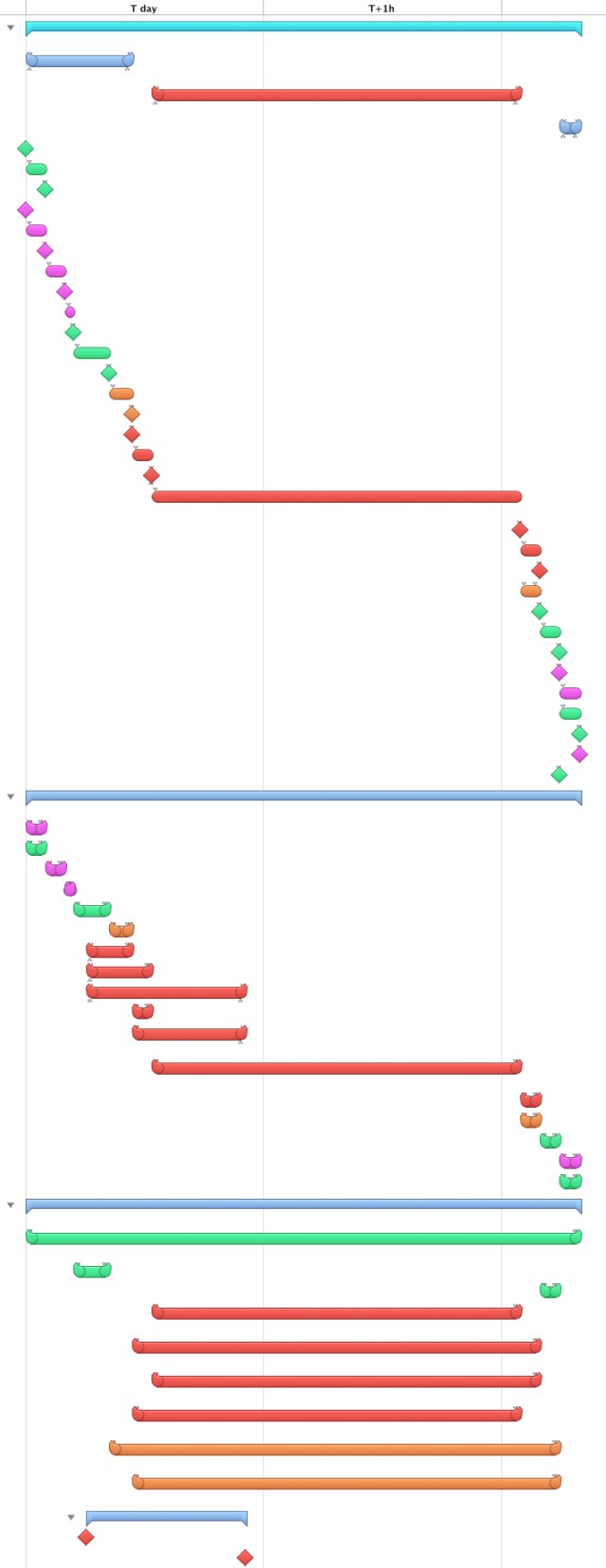
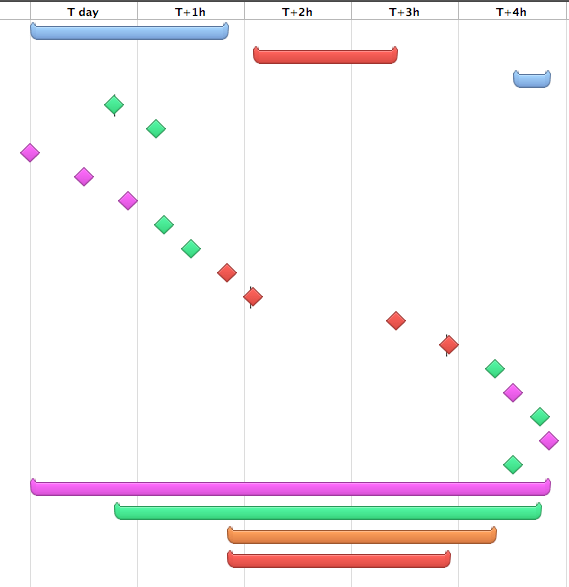
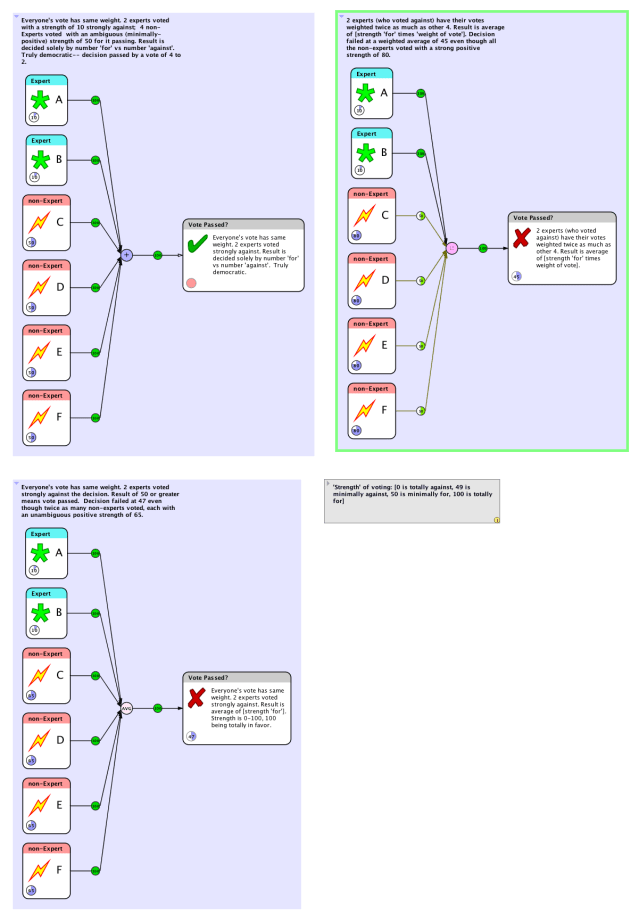
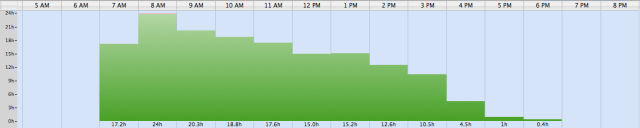
Analytics can be defined as the presentation of input in such a way that it taps into the much broader wealth of knowledge and experience that you hold. Much as a picture of dots lets you see a larger, whole picture, good analytics helps you fill in the dots with what you know from all your theory, prior work, and play.
Analytics creates a loose framework to help integrate your current senses and data with your broader knowledge and appreciation of the context of the situation. Context will effect the interpretation of any sense, and the framework can help in applying the context.
Analytics can be thought of as an aid to intuition. Since intuition is thought of as an assimilation and assessment of thoughts in our subconscious, a loose visual framework can help coach you into understanding your gut feelings without forcing you into a rigid thought process as so many statistics do. Many statistical analyses and their resulting graphics tend to eliminate the context of a situation and decrease the ‘degrees of freedom’ in order to achieve a specific number that gives little help in solving complex problems. For example: The average blood pressure in a hospital is 120/80; does that mean we can discard all the vasopressers, vasodilators, and diuretics?
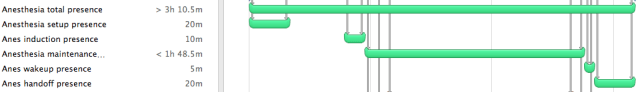
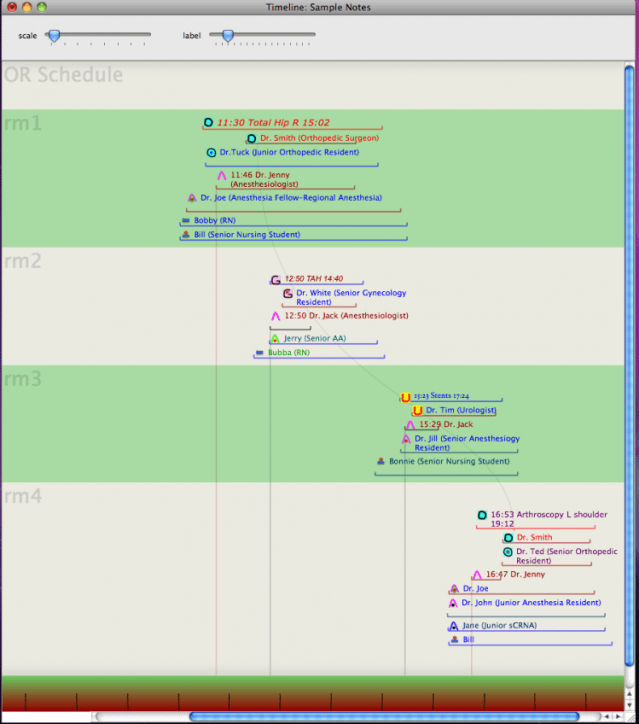
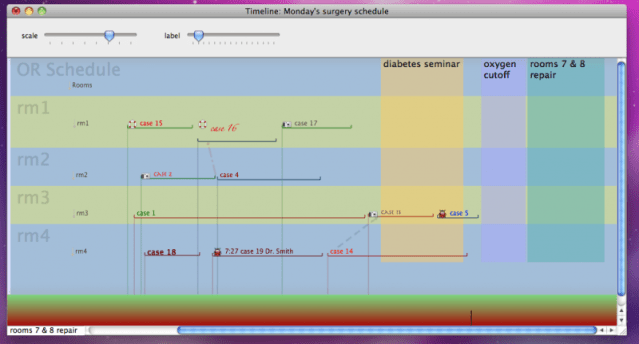
How about the use of numbers from an arterial line or Swan-ganz catheter? A projection of multi-factoral influences onto a two-dimensional axis (arterial tracing, Swan-Ganz numbers) and erroneously discarding the other observations. Too much emphasis on micro-analyzing the subtleties of the two-dimensional projection of a multifactorial effect is a mistake. Concurrent observance of other factors increases understanding and decreases time, cost, and morbidity in finding solutions. The proper analytics can help focus the narrower statistical and invasive analyses to where they do the most good. Experience and theory helps forms the intuition that analytics taps in to.
Visual analytics is common in conversation today. But sight is not the only sense that cues us to understanding a situation.
For example:
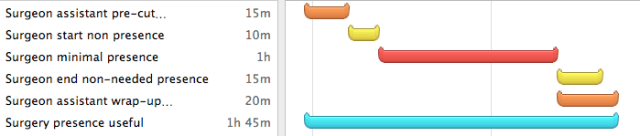
In anesthesia we used to listen to heart and breath sounds with a precordial stethoscope continuously throughout a case. Subtle changes in sound often occurred long before any other signs that something was amiss. Now-a-days we’ve substituted a pulse oximeter and capnography which is both a gain, and a loss, in monitoring a patient.
Baseball combines visual and auditory analytics. An outfielder relies on both to catch a ball.
Noise leading up to a potential car crash.
An expert car mechanic uses auditory and tactile information as much as visual.
A physician feeling pulses, warmth of a limb, and listening to heart sounds…integrative.
A monkey swinging through the trees has excellent kinesthetic and visual analytics.
A trapeze artist has great hand-eye coordination, a combination of kinesthetic and visual analytics.
Gustatory and olfactory analytics permit a good cook to make a savory dish without a cookbook.
Beethoven, the German composer and pianist, had excellent auditory analytics. He knew what sounds went well together. He composed, conducted, and performed even when completely deaf. A child prodigy, in auditory analytics.
Mozart was the same, an excellent composer.
Many mathematicians are musicians.
Einstein was not a great mathematician, although he was a great theorist. His power came from understanding relationships and building frameworks to explain the world even though he needed help to model those relationships mathematically.
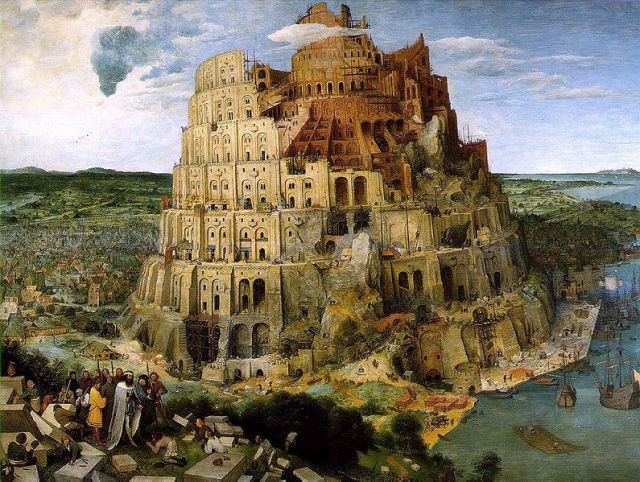
Analytic abilities evolved out of the necessity to survive. Experience is integral to analytics as is theory which is often created from experience. With it we solve problems and see potential.
Analytics help one focus on the important factors and ignore ‘noise’.
A language, when understood well, permits people to slur and leave out words. A foreigner, though he speaks english, can have great difficulty understanding pig-Latin though children do so with ease. When you understand the framework of a language, then ‘noise’ is more tolerable.
And, multiple sense analytics can be fun. Imagine auditory (Bolero) with olfactory (lavender) with visual (lace) with tactile (massage oil).
With Visual Analytics, the more you know the more you’ll see… and the more you’ll know.