Excess CRNA Hours $900,000 waste a year
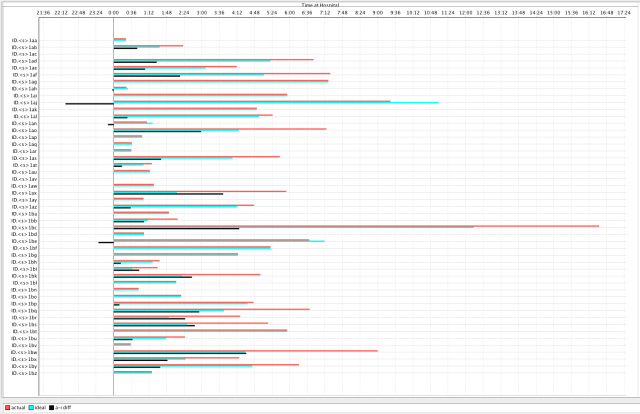
<click on graph to enlarge in separate window> [Note that the scale for the upper and lower graphs are different]
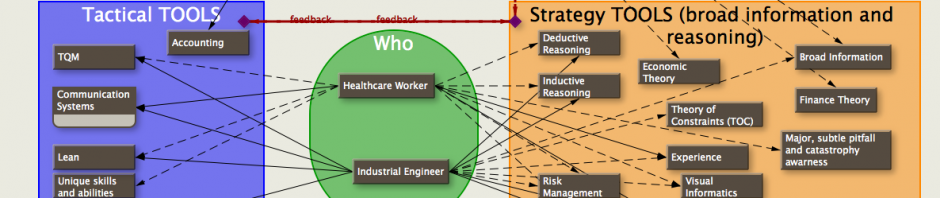
I mentioned in the prior post that my client had wanted an analysis of how well they were using their CRNAs. By using the time sheets for the CRNAs, and the data from the anesthesia records, I came up with these two graphs.
The top graph shows times from the anesthesia records—the times that the CRNAs were doing cases (revenue for the anesthesia group).
The bottom graph shows the times the CRNAs were at the facility and being paid (expense for the anesthesia group). The red part of the graph shows how many extra CRNAs present that were not needed during the peak hours.
(I suggest clicking on the chart which will enlarge it in another window so that you can more easily follow the description and analysis. Both graphs are scaled the same. The actual hours used and hours available are at the bottom of each graph.)
Assuming the initial room preparation time by a CRNA of under an hour, there should be no more CRNAs present the hour before the first cases start than there are during the subsequent hour they are actually doing those cases. There are 12.3 CRNAs available from 6 am to 7am, but only 8.8 CRNAs doing cases from 7 am to 8am which is [(12.3-8.8 =3.5)]; 3 CRNAs too many. From 7 am to 8 am there are 23.7 CRNAs, but only 16.1 CRNAs doing cases from 8 am to 9 am [(23.7-16.1)=7.6]; 7 CRNAs too many. The rest of the peak hours also show from 5 to 11 more CRNAs present than needed. From 2 pm to 4 pm there’s an appropriate amount of CRNAs present for the case load. However, from 4 pm to 7 pm there are too many CRNAs.
Other important data is that the CRNAs are paid overtime after 40 hours of work in a week—there’s no overtime on a daily basis; the case scheduling is done by the nurses, not the anesthesiologists, and the anesthesiologists are guaranteed a minimum income which is just above what they would earn from the cases themselves.
While discussing the situation with my client, he said that a rough estimate of costs for 5 CRNAs a year would be close to $900,000. Looking at the graphs, even with the current system for scheduling cases and not adjusting anyone’s work schedule, they could conservatively have 5 fewer CRNAs for the entire normal work day without making lack of CRNAs the constraint in the OR. That’s $900,000 a year that if divided among a group of 25 anesthesiologists a year would be valued at $36,000 per anesthesiologist per year. If you then add the extra CRNAs that are around from 4 pm to 7 pm [(8.9-4.9)+(8.5-4.3)+(5.8-3.8)=10.2]; you add an additional 10 hours of CRNAs not needed.
Depending on how conservative you want to be in your calculations, just with better scheduling they could hire 5 to 7 fewer CRNAs and save between $36,000 to $42,400 per year for each of the 25 anesthesiologist. If there were only 20 anesthesiologists, this would save up to $53,000 per year per anesthesiologist; this increase in income is in addition to the [25/20=1.25] 25 percent increased income due to dividing the revenue among fewer anesthesiologists.
Why don’t they schedule the CRNAs better? One reason is they lose track of their CRNAs—and they aren’t aware of the easy and inexpensive ways to tightly coordinate their activities with modern technology. Another reason is hospital politics.
Where things get really exciting is when the anesthesiologists control the schedule. This is possible when the anesthesiology group has an exclusive contract with the hospital, common in the southeastern US but not allowed in some other states. Even where exclusive contracts aren’t permitted, there is still a way to simulate the incentives and gains that can come with an exclusive contract. More on that later…